Herniated Disc / Bulging Disc / Protruding Disc – Overview
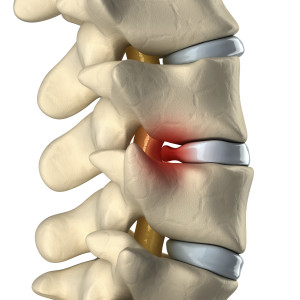 When your back hurts – your day to day activities can become unbearable. Just sitting, bending or twisting can cause sharp pain, dull aches or numbing and tingling. A main cause to these symptoms is a herniated, bulging or protruding disc, also sometimes referred to as a ruptured disc. The spine is made up of many vertebrae which are stacked upon one another, and in between each of these bones are discs. These discs are the spines shock absorbers. As a person ages, these discs progressively and naturally become less supple and more fragile and can herniated, bulge or protrude causing pain and discomfort. Discs can herniate in any direction–forward, centrally or, most commonly, backward and sideways in the direction of the spinal nerves. They are sometimes referred to as “slipped discs” yet this is not an appropriate term, because discs do not ever slip out of placement, as they are attached by tissue to the vertebrae both above and below. A bulging or protruding disc forms when the wall of the disc is deformed but not necessarily herniated. The nucleus is still contained in the wall. Common causes of this condition are aging, excessive heavy lifting, and in more rare cases – a traumatic event such as a fall or accident. There are also many other factors that can put a person into a higher risk of susceptibility for the condition, such as smoking, excess weight, diabetes, and having an occupation that strains the spine.
When your back hurts – your day to day activities can become unbearable. Just sitting, bending or twisting can cause sharp pain, dull aches or numbing and tingling. A main cause to these symptoms is a herniated, bulging or protruding disc, also sometimes referred to as a ruptured disc. The spine is made up of many vertebrae which are stacked upon one another, and in between each of these bones are discs. These discs are the spines shock absorbers. As a person ages, these discs progressively and naturally become less supple and more fragile and can herniated, bulge or protrude causing pain and discomfort. Discs can herniate in any direction–forward, centrally or, most commonly, backward and sideways in the direction of the spinal nerves. They are sometimes referred to as “slipped discs” yet this is not an appropriate term, because discs do not ever slip out of placement, as they are attached by tissue to the vertebrae both above and below. A bulging or protruding disc forms when the wall of the disc is deformed but not necessarily herniated. The nucleus is still contained in the wall. Common causes of this condition are aging, excessive heavy lifting, and in more rare cases – a traumatic event such as a fall or accident. There are also many other factors that can put a person into a higher risk of susceptibility for the condition, such as smoking, excess weight, diabetes, and having an occupation that strains the spine.
Your spinal column is made up of bones (vertebrae) that are cushioned by small disks consisting of a tough outer layer (annulus) and a soft, jelly-like inner layer (nucleus). These disks act as shock absorbers, protecting the spine and nerves from the stress of everyday tasks as well as strenuous work such as heavy lifting. When a disk herniates, a tear or weakness in the annulus allows the jelly-like nucleus to push out into the spinal canal. If it puts pressure on a spinal nerve, the herniated disk can cause pain, numbness or weakness in the back, legs or arms, depending on where the disk is located.
Herniated disks are most common in the lower (lumbar) spine, but about 10 percent occur in the neck (cervical spine). Anyone can get herniated disks, but herniations in the lumbar spine are most common between 35 and 45 years of age. Cervical disk herniation is more common between 50 and 60 years of age.
Herniated Disc / Bulging Disc / Protruding Disc – Symptoms
Because nerve roots act as message lines to other parts of the body, a common difficulty of disc herniation is that it can cause pain that is felt in other parts of the body. For example, leg pain below the knee can often be a symptom of a herniated disc. This type of pain is called radicular pain or radiculopathy. Other common symptoms are:
- Sciatica –aching pain with occasional numbness and tingling. Most commonly, this pain starts in the buttocks and extends down the back of the leg.
- Pain, numbness and/or weakness in the lower back and/or one leg, or pain in the neck, shoulder chest or arm.
- Low back pain that worsens with long periods of sitting, and can also be intensified when sneezing or coughing.
Herniated Disc / Bulging Disc / Protruding Disc – Diagnosis and Treatment
The providers at Michigan Spine & Pain use a variety of methods to diagnose a herniated disc, such as medical history, a complete physical exam, x-rays, MRI, CT scan, electrodiagnostics, bone scans , discography and many other methods. Many patients that are diagnosed with a herniated disc can manage their pain level with traditional methods. At Michigan Spine & Pain, we use the following treatment methods to develop a treatment plan specific to each patient’s needs and condition:
- Physical Therapy. Working with a physical therapist can help build strength and endurance in order to maintain the flexibility and stability of your spine.
- Acupuncture. An acupuncture program can help a patient manage their pain in many cases. Acupuncture is a health science that can be used successfully to treat pain and dysfunction in the body. Acupuncture’s goal is to restore normalcy to the body’s energy balance by utilizing a combination of Acupoints located on the twelve meridians. This can be accomplished by a variety of means, the needle is just one.
- Injections. The epidural space is located between the spine and vertebrae. Medication such as corticsoteriod or local anesthetic is injected into this space by way of a needle. It can block the inflammatory chemicals that sensitize nerves and nerve receptors, and thus in many cases – help to reduce pain.
- Chiropractic Care. Chiropractic care is an important part of our treatment plans at Michigan Spine and Pain. Our medical doctors recognize the benefits of chiropractic care, and work with our chiropractor to reduce pain and improve function quickly.
- Massage Therapy. During a massage, a trained, clinical massage practitioner manipulates muscles in the body. This, combined with a full pain management treatment plan, can provide relief. It is a safe procedure that is only performed by one of Michigan Spine & Pains licensed massage therapists.
- Pain Management. Pain Management is an overall approach and philosophy to treating chronic pain conditions. Medications can be an important part of this approach. All of the physicians at Michigan Spine and Pain are Board Certified and have years of experience with acute and chronic pain conditions.
- Pain Psychology. Pain Psychology/Social Work is integral to our treatment plans. Pain is something our patients experience 24 hours a day, seven days a week. This constant battle is depressing and debilitating. Patients and their families may also have lost income or relationships due to injury or illness. At Michigan Spine and Pain we believe it is important to address these issues along with the physical issues.
- Transcutaneous Electrical Nerve Stimulation (TENS). Electrodes placed the skin near the painful areas deliver tiny electrical impulses that may relieve pain.
Herniated Disc / Bulging Disc / Protruding Disc – Prevention
This condition can be, in many cases, prevented. Some simple steps that can be taken to reduce the risk of developing a herniated disc are:
- Maintain a healthy weight. Excess weight naturally puts more strain on the back and spine. This strain will make the spine more susceptible to herniation or bulging over time.
- Exercise. Regularly exercising can slow the age related degeneration of discs, and can add strength to the core muscles that stabilize the spine.
- Maintain proper / good posture. Posture reduces pressure on the spine. Keeping the back straight, and aligned, especially when sitting for extended periods of time can help reduce the risk for a herniated disc.
- Avoid heavy lifting. When one must lift heavy objects, lifting with the legs, not the back, will help reduce the risk of a herniated disc.